by Connie Hernandez, ND
What is thermal imaging?

Connie Hernandez, ND
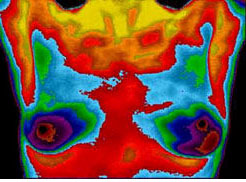
Thermal breast imaging – commonly referred to as breast thermography – is a quick, safe, accurate, non-invasive test that can often detect changes that accompany breast disease earlier than breast self-examination, doctor examination, and even mammography.
The earliest stages of breast cancer are accompanied by changes in breast temperature and blood supply. These changes can often be seen on a thermal image, even before a visible tumor develops.
Our thermal imaging system scans the breasts using an extremely sensitive thermal imaging camera that requires no radiation or breast compression. The resulting images are evaluated by experienced technicians using sophisticated technology to determine if the breasts appear to be at risk for disease.
What are the doctors looking for in a breast thermography photo?
Breast disease alters the breast temperature and the surrounding blood supply, creating reliable signs that are clearly seen on a thermal image. Your doctor is looking for the first signs of any existing or potential problems. Early recognition allows for early treatment and great enhances the chances of a positive outcome.
What is the main difference between breast thermography and mammography?
Mammograms use radiation to distinguish dense anatomical structures consistent with tumor growth.
Thermograms look at physiological changes that accompany breast disease. Thermograms don’t “see tumors.” They detect vascular activity and temperature changes that precede or accompany tumor development and growth.
How often should women get breast thermography?
Early thermal imaging photos give us a baseline from which we can monitor breast health. These comparative studies allow early detection of any suspicious changes.
Thermography is recommended on an annual basis for women 30 and over, but may be recommended at 3- to 6-month intervals when there are suspicious thermograms or other diagnostic readings. Thermography may also be recommended to evaluate the effects of hormone replacement therapy, the efficacy of a given treatment, and to identify any other causes for concern.
What will my thermography report tell me?
Your doctor can use your thermography report to evaluate your risk for breast cancer. According to the indicated level of risk, you may be advised to follow a home program to reduce your risk, or you may be referred to a specialist for an intensive, personalized risk reduction program, or to undergo further diagnostic testing.
What can I learn from my thermogram?
Thermography takes the temperature of the breasts. Temperature differentials may be normal for you, or they may reveal underlying physiologic changes. These changes may reflect infection, inflammation, neurological issues, a hormonal imbalance, or cancer or pre-cancerous conditions. Further thermograms can track changes as your body’s physiology returns to normal.
Are there any limitations or disadvantages with breast thermography?
Breast thermography does not replace mammography. It may not detect slow-growing cancers where the breast temperatures and vascular levels remain largely unchanged.
When breast exams, thermography, and mammography are used as complementary diagnostic techniques, the accuracy rates in detecting breast cancer increase dramatically.
What happens during a breast thermography exam?
 The entire exam takes place behind the privacy of a screen. You will not be directly seen or touched by the clinician. The only discomfort from the exam may be chilliness, as the room needs to be kept at a specific, cool temperature for the pictures to be accurate.
The entire exam takes place behind the privacy of a screen. You will not be directly seen or touched by the clinician. The only discomfort from the exam may be chilliness, as the room needs to be kept at a specific, cool temperature for the pictures to be accurate.
The clinician will instruct you to disrobe from the waist up. You will be asked to sit or stand with your hands on your hips (hands not touching your breasts) for about 15 minutes, while your upper body is scanned.
What are some reputable breast thermography “credentials”?
Digital infrared thermal imaging is recognized as a viable diagnostic tool by the FDA, the AMA Council on Scientific Affairs, the ACA Council on Diagnostic Imaging, the Congress of Neurosurgeons, and the American Academy of Physical Medicine and Rehabilitation.
Restore your Peace of Mind
- Are you concerned that you or a loved one may be at risk for breast cancer?
- Do you wonder if your hormone replacement therapy is increasing your risk for breast cancer?
- Would you feel better if you had a safe, effective way to evaluate how the medicines or supplements you are taking are affecting your breast tissue?
- Are you aware that thermography can actually see the cumulative effect of breast cancer risk variables on your breast tissue?
- Do you know that thermography can monitor the effectiveness of your efforts to reduce your risk of breast cancer?
Breast thermography at Pacific Naturopathic
To determine your thermal risk ratings, we compare temperatures at numerous points on both breasts. At each point, there is a range of temperature variation. When a temperature is outside a normal range at any point, we are alerted – and more alerted when several temperatures are out of range.
An increased temperature differential indicates that there is some kind of process taking place in the hotter breast. The heat may represent injury, infection, inflammation, or abnormal cell growth.
When heat is accompanied by abnormal vasculature, we are further alerted. We may advise a patient in this situation to follow a breast health protocol for three months, and then retest before moving on to anatomic imaging (mammography or ultrasound). Or we may advise immediate further imaging, or even breast biopsy. The course of action will depend on the patient’s unique signs, symptoms, and history.
Breast thermography considerations
Two things come to mind when considering which remedies will most effectively reduce the incidence of breast cancer:
The first is that therapies that help positively change breast physiology are much more likely to succeed than waiting until the physiologic change has created an anatomic change (e.g., a tumor) before trying to do something about it.
Regular thermography readings, over time, allow us to follow any developing physiologic changes and assess whether therapeutic interventions are needed. Mammograms can only tell us that there has already been an anatomic change. Thermography can help us catch the changes before they can be detected on a mammogram. Thermography can then help us track the effectiveness of the chosen therapy.
The second consideration is that when physiologic changes occur, we need to address the underlying cause or causes. These may include imbalanced estrogen and/or progesterone, errors in estrogen metabolism, an iodine deficiency, intake of inflammatory foods, lymphatic congestion (from tight underwire bras, etc.), toxicity of some sort, trauma to the breast, emotional turbulence, or a multitude of other causes.
When these causes are successfully addressed, any high thermal risk ratings on the breast thermography exam will be reduced, indicating that the breast is responding to treatment, and that there will be a corresponding reduced risk of developing breast cancer.
About thermal risk ratings
The thermal risk ratings on your breast thermography report are based on the temperature differentials between the breasts.
A higher temperature at a given location on either breast reflects a physiologic difference in the breast compared to the other breast. The unusual heat reflects metabolic activity that could indicate an injury or other inflammatory processes, or even a developing cancer. In any of these cases, we can be sure that the immune system has been activated and is responding to an issue that it perceives as a health threat.
In addition to treatment protocols that can improve estrogen metabolism (promoting anti-inflammatory metabolites), we may use botanicals to settle down an overactive immune system and support normal immune function.
Typical medicines used to decrease breast inflammation and support breast health include green tea, curcumin, and various mushrooms. After three months of consistent use, we should see a decrease in inflammation and a corresponding decrease in thermal risk rating on subsequent breast thermography exams. If improvement is not seen, we may alter the protocol and/or seek further diagnostics.
The safety of breast health evaluation
It’s clear that women are increasingly reluctant to opt for the annual mammogram, due to a growing awareness that, just as radiation in general has adverse effects on our health, radiating our breasts is not a good idea.
Not that we should never opt for imaging techniques that subject our bodies to radiation, but it’s becoming increasingly clear that we need to choose these techniques with discretion.
A wonderful benefit of thermography is that it offers women a non-harmful, non-invasive way to evaluate breast health, without subjecting the breast to radiation or compression.
What’s the difference between thermography and mammography?
Thermography offers us insights into the active, ongoing functioning of the breast. Mammography offers anatomic imaging.
It stands to reason that these two types of imaging can complement each other – because more information is always better.
When thermography indicates a high risk of breast disease, we may recommend anatomic imaging at our discretion. To help dispel the effects of radiation, we recommend the German drainage remedy Radinex, sold from our pharmacy.
What does “hormonal grade” mean in breast health evaluation?
I often write about the highly useful risk ratings that breast thermography reports can give us. Less often do I write about the very important “hormonal grade.”
The hormonal grade is determined by studying the patterns of the blood vessels in the breast. Its most significant use is to evaluate the sum total of estrogen influence on the breast.
Estrogen influence can come from within the body itself (endogenous) or from environmental sources (exogenous).
Dairy, poultry, and many meats are full of exogenous hormones that our bodies absorb and store when we consume those foods. Also, our modern environment is rife with endocrine disruptors – as found, for example, in plastic water bottles. And we can clearly observe some of their influence in the hormonal grade.
A high hormonal grade may be normal and typical during the estrogenic phase of the menstrual cycle in young women, while a lower grade would be expected in menopausal women.
The hormonal grade offers us a way to evaluate the efficacy of therapies that aim at diminishing estrogen in conditions such as ER+ breast cancer. Of course, when evaluating hormonal grade, we must take account of environment factors and exclude them from our observations.
More on “hormonal grade”
When the “hormonal grade” is high on your breast thermography report, it indicates a high level of estrogen stimulation of the breasts.
Patients sometimes feel that they should avoid estrogenic foods altogether – soy products being high on the list.
Actually, the plant estrogens in estrogenic foods (the list is long, with flax seed and soy products at the top) are far weaker than our own human estrogens. In fact, these plant estrogens compete for binding sites with human estrogens, helpfully lowering estrogen when estrogen is high, and boosting estrogen influence when estrogen is lacking.
Of far greater concern than plant estrogens are the hormones used in raising animal products, which we consume when we drink conventional milks or eat the meat of caged chickens and other feedlot animals.
In addition, we imbibe xenoestrogens from a huge variety of sources in our chemically contaminated environment. Xenoestrogens are a type of xenohormone that imitates estrogen. They can be either synthetic or natural chemical compounds. And they are major contributors to disrupting the hormonal levels in human breast tissue.
Thermography can help us track changes in the vascularity of the breast tissue to determine the effectiveness of the current treatment plan. For example, in women who are being treated for breast cancer with aromatase inhibitors and other medicines designed to lower estrogen levels, we can evaluate their effectiveness by studying thermography reports taken before and after treatment.
A high thermal risk rating – what does it mean?
What does it mean when your thermography report reveals a high thermal risk rating?
Every woman’s body is unique and requires an individualized treatment protocol.
Some women will need to heal any underlying emotional wounds as part of the process of achieving effective treatment. Are there unresolved issues in the father/daughter, mother/son, or partner relationship(s)?
For others, a high risk rating may indicate inflammation due to poor dietary choices, same-sided dental issues, lymphatic congestion from lack of activity or tight clothing, or traumatic injury.
Hormonal imbalances can cause a high thermal risk rating. In these cases, the endocrine glands and the chakras (their energetic counterparts) come into play. Also, the individual woman’s genetic makeup and liver and digestive functioning will be key elements in prescribing a protocol for removing toxic estrogen metabolites and other toxins that may be affecting breast health.
Whatever the cause, breast thermography can help us track the effectiveness of the individualized protocol by comparing vascularization and temperature differences before and after treatment.
Thermograms and mammograms provide different information
As with any other lab tests, the usefulness of breast imaging depends on the reliability of the imaging technique. What is the breast thermography (or other analytic instrument) actually seeing?
Mammograms, ultrasounds, and MRIs detect anatomic changes – they’re good at seeing lumps and bumps. But the mammogram’s value is limited for women with dense breasts. And ultrasounds are used primarily to discriminate cysts from solid masses.
MRIs offer the most precise detection, but because they are expensive, they are generally reserved for women with high-risk histories and other special conditions.
Thermograms detect physiological differences in temperature and vascularity between the breasts. The density of the breast tissue does not affect the accuracy of thermographic testing.
As I mentioned earlier, taking before-and-after thermograms lets us detect any physiological differences from one thermogram to the next. For example, we can take thermograms before and after treatment with a given breast health protocol to evaluate its efficacy.
We can also assess the effect of estrogens on the breasts – a very helpful tool for women taking hormone replacement or anti-estrogen therapy.
Advantages of thermography over mammography
Thermography helps us understand developing situations in the breast tissue that would not show up on a mammogram until much later. It’s important to note that neither mammograms or thermograms can diagnose breast cancer, and that neither can uncover a potential breast cancer with 100-percent accuracy.
Changes in blood flow and “hot spot” temperature changes will always precede any physical changes (lumps and bumps). Still, for the best possible diagnosis, it’s often helpful and even essential to have both anatomic and physiologic data.
****






Speak Your Mind
You must be logged in to post a comment.